Advanced Non‐Squamous Non–Small Cell Lung Cancer
How is NSCLC detected in terms of presence?
While early stages of lung cancer often go undetected, lung cancers are at times detected incidentally as a part of unrelated medical tests.
While early stages of lung cancer often go undetected, lung cancers are at times detected incidentally as a part of unrelated medical tests. Most NSCLC patients are currently detected at advanced stages.
To check for cancer, tissue or fluid must be removed from the lungs. There is no single-point method identified yet that fits all. Diagnosis and detection of lung cancer is based on signs, symptoms and laboratory tests, aided by imaging. Usually recommended diagnostic and detection methods involve:
- During bronchoscopy, the doctor threads an instrument called bronchoscope through the airways to see the inside of the lungs. Often, ultrasound is clubbed with bronchoscopy (‘Endobronchial ultrasound (EBUS)’) for better outcome.
- Image-guided Transbronchial needle aspiration (TBNA) is a recommended technique to extract lung tissue samples for biopsy. These tissue samples can then be tested for predictive and prognostic molecular markers such as EGFR overexpression, EGFR T790M mutation, KRAS and ALK by immunohistochemistry (IHC) (click here for IHC). To know more on why test for these markers, click here.
- Sputum cytology requires that the patient cough up some phlegm, which is then tested for cancer cells. This may be the easiest test to perform, but is not sufficient to confirm absence of cancer.
- During external needle biopsy cells from peripheral cancer lesions can be aspirated for biopsy. This method has an acceptable rate of diagnostic accuracy
- More invasive, surgical methods may also be also considered when the above-described techniques cannot allow for an accurate diagnosis.
- Immunohistochemistry (IHC) is a WHO recommended method for detection of predictable markers and diagnosis of lung cancer. During IHC, selected protein(s) in cells are identified by specialized staining called immunostaining.
How is extent of spread detected?
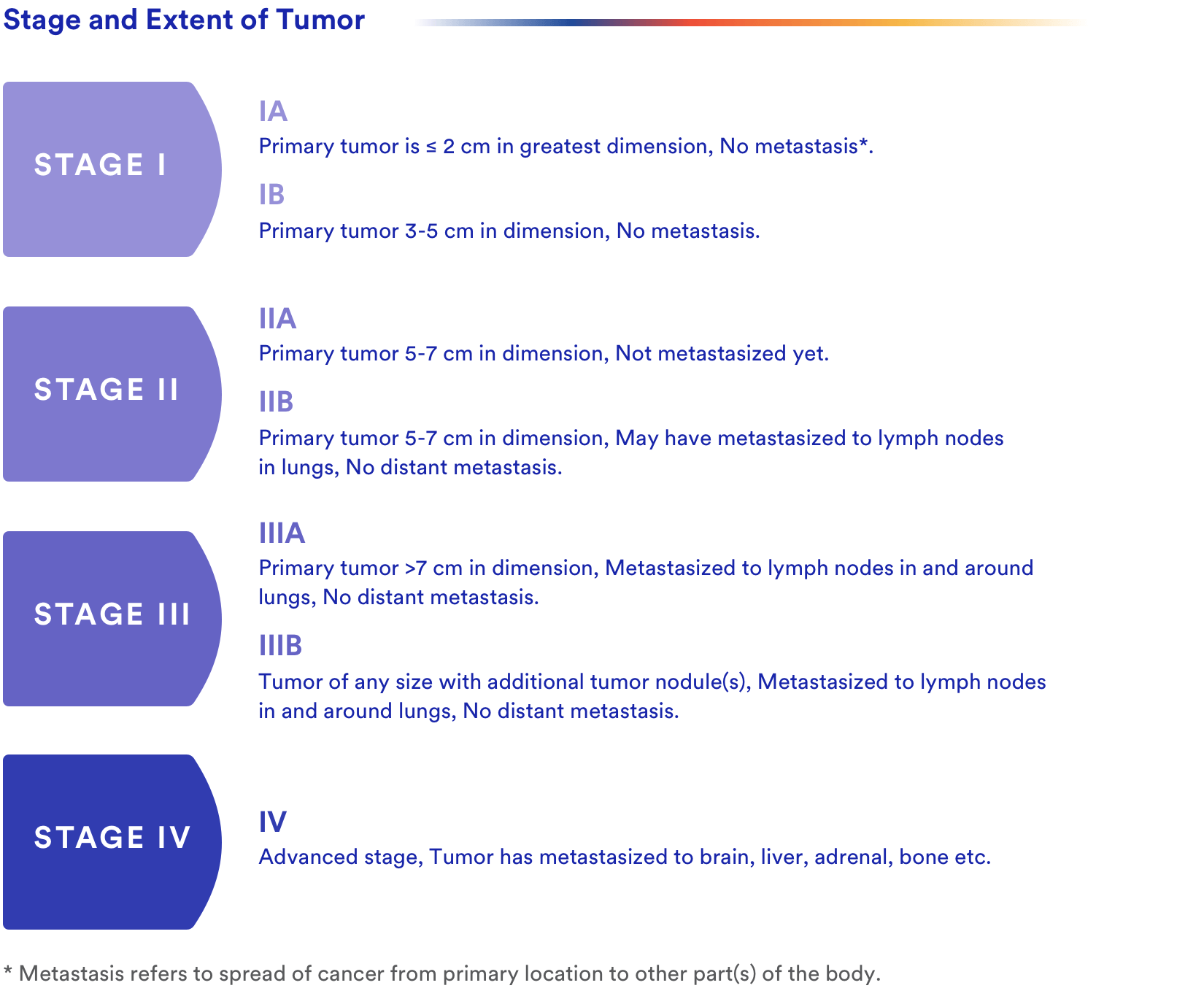
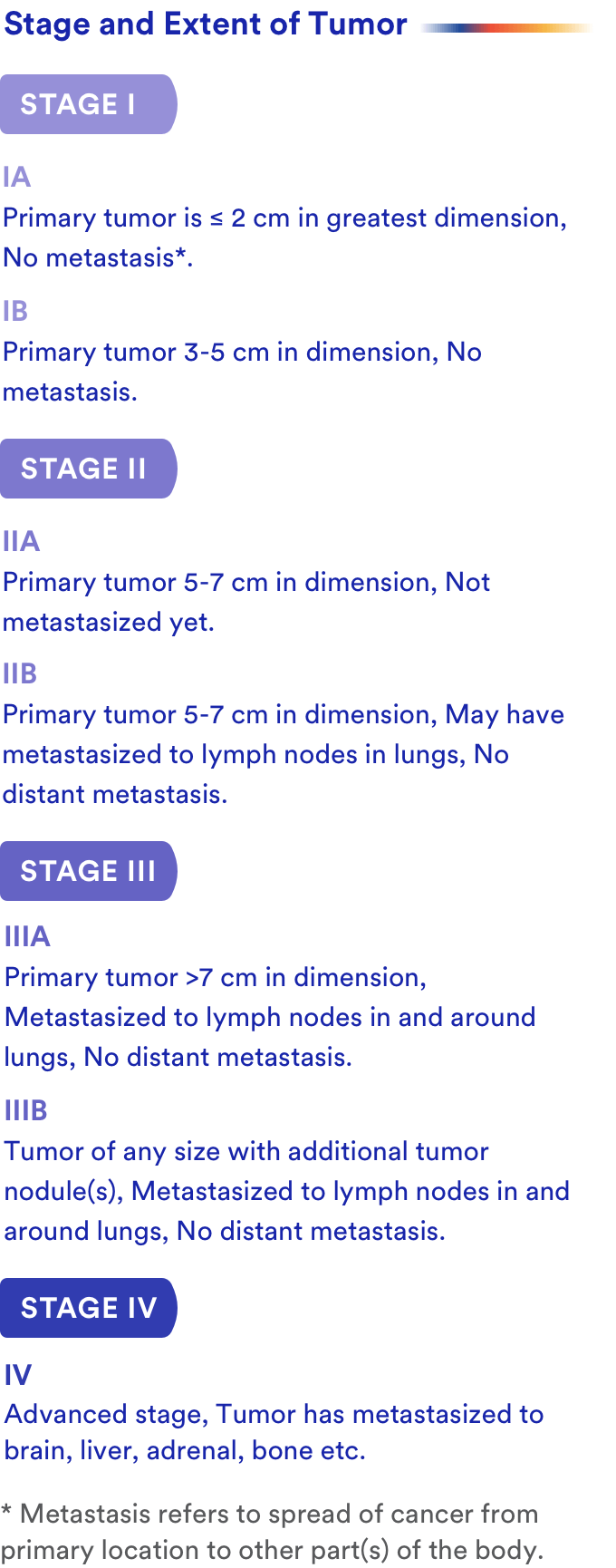
Accurate staging of cancer helps the doctor devise the best possible treatment regimen in a given case. Staging is done according to the tumour, node, metastasis (TNM) staging system. A quick summary of indicator or each stage of the disease based on the TNM staging is shown in Table 1:
Abbreviations
AJCC: American Joint Committee on Cancer CT scan: Computed Tomography scan EBUS: Endobronchial ultrasound EGFR: Epidermal Growth Factor Receptor IASLC: International Association for the Study of Lung Cancer IHC: Immunohistochemistry IUAC: International Union Against Cancer NSCLC: Non-small cell lung cancer MRI scan: Magnetic resonance imaging scan PET scan: Positron emission tomography scan RFA: Radiofrequency ablation SCLC: Small Cell Lung Cancer SVC: Superior vena cava TBNA: Transbronchial needle aspiration TNM: Tumor, node, metastasis staging system VATS: Video-assisted thoracic surgery VEGF: Vascular Endothelial Growth Factor
References
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394-424. doi:10.3322/caac.21492
- National Cancer Institute, General information about NSCLC, https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq. Updated on 31st August, 2018, Accessed on 14th January 2019
- American Cancer Society, Anatomy of the lung, Available at: https://www.cancer.org/cancer/small-cell-lung-cancer/about/what-is-small-cell-lung-cancer.html
- Jemal, A., Thun, M. J., Ries, L. A., Howe, H. L., Weir, H. K., Center, M. M., Ward, E., Wu, X. C., Eheman, C., Anderson, R., Ajani, U. A., Kohler, B., … Edwards, B. K. (2008). Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. Journal of the National Cancer Institute, 100(23), 1672-94.
- Asomaning, K., Miller, D. P., Liu, G., Wain, J. C., Lynch, T. J., Su, L., & Christiani, D. C. (2008). Second hand smoke, age of exposure and lung cancer risk. Lung cancer (Amsterdam, Netherlands), 61(1), 13-20.
- Hubaux, R., Becker-Santos, D. D., Enfield, K. S., Lam, S., Lam, W. L., & Martinez, V. D. (2012). Arsenic, asbestos and radon: emerging players in lung tumorigenesis. Environmental health : a global access science source, 11, 89. doi:10.1186/1476-069X-11-89
- Cooper, W., Lam, D., O’Toole, S., & Minna, J. (2013). Molecular biology of lung cancer. Journal Of Thoracic Disease, 5(5), S479-S490. Retrieved from http://jtd.amegroups.com/article/view/1597
- American Cancer Society, Non-Small Cell Lung Cancer Signs and Symptoms, Available at: https://www.cancer.org/cancer/non-small-cell-lung-cancer/detection-diagnosis-staging/signs-symptoms.html Accessed on: 14th Jan 2018
- Gould, M. K., Tang, T., Liu, I. A., Lee, J., Zheng, C., Danforth, K. N., … Suh, D. E. (2015). Recent Trends in the Identification of Incidental Pulmonary Nodules. American Journal of Respiratory and Critical Care Medicine, 192(10), 1208-1214. doi:10.1164/rccm.201505-0990oc
- Planchard, D., Popat, S., Kerr, K., Novello, S., Smit, E. F., & Faivre-Finn, C. (2018). Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Annals of Oncology, 29(Supplement_4), iv192-iv237. doi:10.1093/annonc/mdy275
- Adams, K., Shah, P. L., Edmonds, L., & Lim, E. (2009). Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: systematic review and meta-analysis. Thorax, 64(9), 757-762. doi:10.1136/thx.2008.109868
- International Agency for Research on Cancer. (2015). Who Classification of Tumours of the Lung, Pleura, Thymus and Heart. Geneva, Switzerland: World Health Organization.
- Boffa, D. J. (2018). The Eighth Edition Lung Cancer Stage Classification. Lung Cancer: A Practical Approach to Evidence-Based Clinical Evaluation and Management, 57-66. doi:10.1016/b978-0-323-48565-4.00003-5
- Source of information: Classification information & library of images collated based on guidelines by the International Association for the Study of Lung Cancer (IASLC), the International Union Against Cancer (IUAC) & the American Joint Committee on Cancer (AJCC) hosted by CHEST, American College of Chest Physicians http://staginglungcancer.org/calculator Accessed on 17th January, 2019
- American Cancer Society, How is non-small cell lung cancer treated? Available at: https://www.cancer.org/cancer/non-small-cell-lung-cancer/treating.html Accessed on 17th January 2019
- Filosso, P. L. (2011). Emerging treatment options in the management of non-small cell lung cancer. Lung Cancer: Targets and Therapy, 11. doi:10.2147/lctt.s8618
- Jemal, A., Thun, M. J., Ries, L. A., Howe, H. L., Weir, H. K., Center, M. M., Ward, E., Wu, X. C., Eheman, C., Anderson, R., Ajani, U. A., Kohler, B., … Edwards, B. K. (2008). Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. Journal of the National Cancer Institute, 100(23), 1672-94.
- Asomaning, K., Miller, D. P., Liu, G., Wain, J. C., Lynch, T. J., Su, L., & Christiani, D. C. (2008). Second hand smoke, age of exposure and lung cancer risk. Lung cancer (Amsterdam, Netherlands), 61(1), 13-20.
- Problems after surgery, Cancer Research UK, Available at: https://www.cancerresearchuk.org/about-cancer/lung-cancer/treatment/surgery/possible-problems Accessed on 21-01-2019